Blue Shield of California, Salesforce Making Prior Authorization as Simple as Using a Credit Card
- Nonprofit health plan's prior authorization platform solution built on Salesforce Health Cloud will work within physician systems to gather relevant clinical data from electronic health records and streamline 20+ disparate systems; members and physicians will get prior authorization in near real-time
- Testing begins in early 2025 with limited rollout later in year; near real-time prior authorization available January 2026; additional capabilities to follow
OAKLAND, Calif., Oct. 21, 2024 /PRNewswire/ -- Blue Shield of California and Salesforce (NYSE: CRM), the #1 AI CRM, are teaming up to solve a significant healthcare challenge — providing physicians and their patients prior authorization answers in near real-time, rather than days. Together, Blue Shield and Salesforce will make prior authorization simpler, faster and more transparent. The platform solution, which will be built on Salesforce Health Cloud, will also connect members to personalized health support by automatically alerting care teams of prior authorization requests.
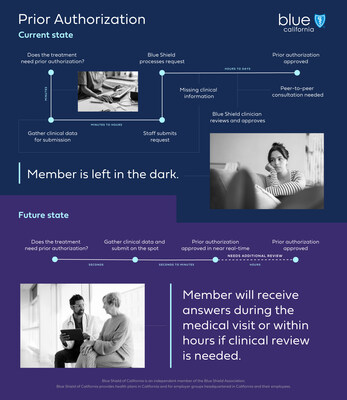
Health plans rely on prior authorization to ensure certain recommended treatments and services are safe, evidence-based and high-value for their members. However, according to the American Medical Association's annual survey, 78% of physicians said issues with prior authorization can lead to patients foregoing care. This is in part due to outdated and inefficient healthcare industry processes:
- About two-thirds of prior authorization requests are submitted manually or partially manually, including by fax machine.
- Submissions that lack complete clinical information slow the process.
- Outdated electronic systems waste time and resources.
- All the while, patients are left without answers, worried about their next steps in care.
Blue Shield will use Health Level Seven (HL7) Fast Healthcare Interoperability Resources (FHIR) standards to create technology that will streamline 20+ disparate systems that exist today into one process that integrates with physicians' current workflow.
Future Experience Will Be Fast, Efficient and Easy
Prompted by the physician, the platform solution will search a patient's electronic health record for relevant clinical information and compile it into a pre-populated electronic form. Physicians will be able to submit requests from their systems on the spot — no fax machine needed — and members will receive answers during their medical appointments. Modifications or denials will always be made by a medical director or licensed clinician.
A small number of cases may require clinical consultation. When that happens, physicians will receive a message in near real-time detailing what is needed to complete the authorization, and options to begin a peer-to-peer clinical consultation. This currently can take several days. In the future, this can happen within hours, depending on the requesting physician's availability. Throughout this process, members will receive status updates in their Blue Shield member app, giving them a new level of transparency.
"Prior authorization was never meant to be a barrier or a burden. As a health plan, it's our responsibility to ensure safe, evidence-based, high-value care for our members, and we know it can be an easier process for everyone," said Paul Markovich, chief executive officer, Blue Shield of California. "That's why we are taking the bold step to make it as easy as using your credit card, while enabling more coordinated, personalized support for members. It is time for the industry to let go of fax machines."
"For years, we've heard that technology will be the answer to systemic issues in health care, but few solutions have made a scalable impact," said Jeff Amann, executive vice president and general manager, Salesforce Industries. "With Blue Shield of California, we're rebuilding the prior authorization process with new innovations that support near real-time decision-making so providers can more quickly, transparently and compliantly deliver the attentive care their patients deserve."
Moving the Healthcare Industry Forward
Blue Shield will go beyond current efforts in this space: the Centers for Medicaid and Medicare Services' Interoperability and Prior Authorization Final Rule requirements; efforts by health plans that focus on reducing the number of treatments that require prior authorization; and gold carding, which removes prior authorization for physicians that meet certain requirements for a set period of time.
"As a practicing physician, I'm proud that we're taking on this challenge to build a solution that allows providers to focus on delivering care — why they became physicians in the first place — rather than adding to the administrative burden," said Ravi Kavasery, M.D., chief medical officer, Blue Shield of California.
Enabling More Holistic, Comprehensive Care
The new platform solution will work alongside Care Connect — Blue Shield's care management system — creating a clinical infrastructure that shifts the focus from the moment of medical necessity to ongoing, preventive care and wellness. In the future, a prior authorization request will automatically alert the health plan's team of nurses, social workers and behavioral health specialists that a member may need new or increased health support.
For example, if a physician requests approval for a continuous glucose monitor, care teams are automatically prompted to contact the member with information on diabetes reversal programs available through their Blue Shield benefits. In this way, prior authorization enables members to get more personalized, coordinated care.
Creating a Healthcare System Worthy of Family and Friends
This is Blue Shield's latest bold move to reimagine health care. In 2023, the health plan announced Pharmacy Care Reimagined, its groundbreaking model to transform prescription drug care. Earlier this month, Blue Shield announced a collaboration to slash the cost of the world's best-selling drug, Humira. Blue Shield has developed new payment models in collaboration with physician and hospital partners to bring better value into the healthcare market and bend the cost of health care trend. By the end of 2024, all members will have access to their health information through Blue Shield's Member Health Record.
About Blue Shield of California
Blue Shield of California strives to create a healthcare system worthy of its family and friends that is sustainably affordable. The health plan is a tax paying, nonprofit, independent member of the Blue Shield Association with more than 4.8 million members, over 7,100 employees and more than $25 billion in annual revenue. Founded in 1939 in San Francisco and now headquartered in Oakland, Blue Shield of California and its affiliates provide health, dental, vision, Medicaid and Medicare healthcare service plans in California. The company has contributed more than $77 million to the Blue Shield of California Foundation in the last three years to have an impact on California communities.
For more news about Blue Shield of California, please visit news.blueshieldca.com.
Or follow us on LinkedIn or Facebook.
CONTACT: Amanda Wardell
Blue Shield of California
510-607-2359
media@blueshieldca.com
![]() View original content to download multimedia:https://www.prnewswire.com/news-releases/blue-shield-of-california-salesforce-making-prior-authorization-as-simple-as-using-a-credit-card-302281219.html
View original content to download multimedia:https://www.prnewswire.com/news-releases/blue-shield-of-california-salesforce-making-prior-authorization-as-simple-as-using-a-credit-card-302281219.html
SOURCE Blue Shield of California